How telehealth is shaping the future of medicine
The healthcare field has experienced a transformative shift with the growth of telehealth and telemedicine. These technologies are bridging the geographical gap between patients and healthcare providers, opening up new avenues for accessible and convenient medical care.
In this article, we'll explore the definitions of telehealth and telemedicine. We will provide insights into how telehealth operates, delve into the benefits it offers, and explore examples that illuminate its potential to fundamentally alter the way medical care is sought, delivered, and experienced.
What is telehealth?
Telehealth refers to the use of digital communication technologies to provide healthcare services remotely. It encompasses a wide range of digitally enabled methods and tools that allow patients and healthcare providers to interact, consult, diagnose, treat, and manage medical conditions without the need to occupy the same physical space. Telehealth leverages various communication channels, such as video conferencing, phone calls, messaging apps, and data-sharing platforms, to facilitate virtual medical consultations and health-related interactions.
The primary goal of telehealth is to bridge geographical and logistical barriers, enabling individuals to access medical care and expertise irrespective of location. This technology has gained significant traction due to its potential to enhance healthcare accessibility, reduce costs, and improve patient outcomes. It is particularly valuable in situations where in-person visits are challenging, time-consuming, or not immediately required.
In essence, telehealth leverages modern communication tools to transcend traditional healthcare delivery requirements, bringing medical expertise to the digital realm and transforming the way patients and healthcare providers interact and collaborate.
What is telemedicine?
Telemedicine refers to the practice of delivering clinical healthcare services remotely through the use of communication technology. It involves the use of telecommunications tools and digital platforms to enable healthcare providers to diagnose, treat, and manage patients' medical conditions from a distance. Telemedicine is a subset of the broader concept of telehealth, focusing specifically on the clinical aspect of healthcare delivery.
Telemedicine encompasses a variety of medical services that can be provided remotely, including:
Virtual consultations
Virtual consultations bring patients and healthcare professionals together through video conferencing or phone calls. Patients can discuss symptoms, receive diagnoses, and get treatment recommendations, all without the need for an in-person visit. This approach is particularly useful for non-urgent medical concerns or routine check-ups.
Virtual consultation example
Imagine a patient experiencing persistent headaches. Instead of traveling to a clinic, they can schedule a virtual consultation with a neurologist. The neurologist evaluates their symptoms and recommends further tests, lifestyle changes, or potential treatments, providing personalized guidance remotely.

Prescription management
With telemedicine, healthcare providers can assess a patient's condition remotely and prescribe necessary medications. Prescriptions can be sent electronically to the patient's preferred pharmacy, eliminating the need to physically collect paper prescriptions.
Prescription management example
A patient with a sinus infection consults a telemedicine provider. After evaluating their symptoms and medical history, the provider determines that antibiotics are necessary. They electronically send the prescription to the patient's local pharmacy, minimizing the time and travel required for a patient to access needed medication.
Follow-up care
Telemedicine enables patients to receive follow-up appointments and consultations after undergoing treatments or procedures. This eliminates the need for them to return to a physical clinic, making it convenient for both patients and healthcare providers (likely increasing follow-up compliance in the process).
Follow-up care example
A patient who recently underwent minor surgery needs a follow-up appointment to assess their healing progress. Instead of traveling back to the hospital, they have a virtual follow-up with their surgeon. The surgeon examines the incision site, answers the patient's questions, and adjusts their care plan if needed.
Specialist consultations
Telemedicine breaks down geographical barriers by allowing patients to consult with specialists from various medical fields without the need for travel. This is particularly valuable for individuals facing rare or complex conditions.
Specialist consultation example
A patient in a rural area requires input from an oncologist about a suspected rare form of cancer. Through telemedicine, the patient and their local doctor connect with the oncologist. The oncologist reviews the patient's medical history, test results, and imaging remotely, providing expert insights and recommendations for further evaluation.
Monitoring chronic conditions
Telemedicine offers remote monitoring of chronic conditions through wearable devices and home monitoring equipment. This allows healthcare providers to track patients' health metrics and intervene if any irregularities are detected.
Monitoring chronic conditions example
A diabetic patient uses a continuous glucose monitoring device that sends real-time glucose readings to their healthcare provider. If the readings indicate unstable blood sugar levels, the provider can remotely adjust the patient's insulin regimen and provide guidance to stabilize their condition.
Mental health support
Mental health professionals leverage virtual platforms to conduct therapy sessions and offer counseling services. Telemedicine makes it easier for individuals to access mental health support discreetly and conveniently.
Mental health support example
A person struggling with anxiety and depression schedules a virtual therapy session with a licensed psychologist. During the session, they discuss their concerns, learn coping strategies, and receive emotional support, all from the comfort of their home.
These practical examples illustrate how telemedicine services enhance healthcare accessibility, improve patient experiences, and enable healthcare professionals to deliver effective care remotely.
It's important to note that telemedicine doesn't replace all in-person healthcare interactions, but rather complements them by providing an alternative means of accessing medical services, especially for non-emergency situations.
As touched upon earlier, telehealth and telemedicine are closely related terms, but they have distinct meanings within the realm of healthcare. While they are often used interchangeably, there are subtle differences that set them apart:

Telehealth vs. telemedicine
Telehealth serves as the umbrella term that covers both clinical and non-clinical healthcare activities delivered remotely, while telemedicine specifically refers to the remote clinical services that healthcare providers offer to diagnose, treat, and manage patients' medical conditions.
Telehealth covers not only the clinical diagnosis and treatment provided by telemedicine, but also refers to health-related education, administrative functions, and other health services facilitated by technology. Telehealth focuses on promoting overall health and wellness beyond just clinical care.
Some of the key differences between telehealth and telemedicine include:
Scope of services
- Telehealth: Encompasses a wider scope of services, including non-clinical activities like health education, administrative tasks, and remote monitoring.
- Telemedicine: Focuses exclusively on clinical care, involving medical diagnosis, treatment, and management through remote communication.
Clinical vs. non-clinical
- Telehealth: Includes both clinical and non-clinical services aimed at promoting general health and well-being.
- Telemedicine: Specifically addresses clinical aspects of healthcare, dealing with medical diagnosis, treatment, and patient care.
Applications
- Telehealth: Applicable to a broad range of healthcare activities, such as health education, administrative tasks, and remote monitoring.
- Telemedicine: Specifically applied to the remote delivery of medical care and services, involving consultations, diagnoses, and treatment.
Focus
- Telehealth: Focuses on the holistic approach to healthcare, considering various aspects of wellness and health management.
- Telemedicine: Focuses on providing medical care remotely, addressing specific health conditions and medical concerns.
Benefits of telehealth
As telehealth continues to evolve, its benefits ripple across patients' lives, healthcare providers' workflows, and the broader healthcare landscape. With its potential to democratize medical care, improve patient outcomes, and streamline healthcare services, telehealth aims to harness the synergy between technology and healthcare expertise.
In this section, we will explore how telehealth technology transforms healthcare for the better:
Accessibility
Telehealth can help break down the formidable geographical barriers that once hindered individuals from receiving timely medical attention. Patients residing in remote or underserved areas can now connect with healthcare providers, regardless of their physical location.
Convenience
Thanks to telehealth, patients with the ability to navigate digital tools can access medical advice, receive prescriptions, and partake in follow-up consultations with relative ease. Consider a busy professional who can now consult with a doctor during a lunch break, negating the need to disrupt their workday for a routine medical appointment.
Cost savings
Telehealth's financial advantages are twofold. Patients can considerably cut down on transportation costs, eliminating the need to travel to medical facilities. Furthermore, the time saved from reduced travel directly translates to fewer hours away from work, which can be especially advantageous for those who rely on hourly wages. Additionally, healthcare systems benefit from reduced overhead costs as the need for physical infrastructure and resources is minimized.

Improved chronic disease management
Remote patient monitoring (RPM), a cornerstone of telehealth, plays a pivotal role in the continuous and proactive management of chronic conditions. Patients grappling with conditions such as diabetes, hypertension, or heart disease can wear specialized devices that track their health metrics continuously. Should an anomaly arise, healthcare professionals are alerted in real-time, allowing for swift interventions. This data-driven approach not only improves patients' quality of life but also contributes to better long-term outcomes.
Reduced healthcare burden
Telehealth serves as a strategic tool to alleviate the mounting burden on healthcare facilities, particularly in situations where non-emergency cases inundate clinics and hospitals. By offering an alternative channel for healthcare delivery, telehealth enables medical professionals to focus on critical cases, reducing wait times, and ensuring that resources are efficiently allocated. This is particularly evident during outbreaks, as telehealth can play a pivotal role in containing the spread of infectious diseases by allowing patients to receive medical guidance from the safety of their homes.
Practical applications of telehealth services
Telehealth's practical applications are as diverse as the medical landscape itself. It empowers patients to actively engage in their healthcare journeys, while also offering medical professionals innovative tools to provide personalized care.
Through these applications, telehealth has reimagined conventional healthcare delivery, creating an ecosystem where medical expertise converges with modern technology to forge a new era of accessible, patient-centric healthcare.
In this section, we uncover the practical applications of telehealth across various medical fields:
Primary care
Telehealth has breathed new life into primary care, revolutionizing routine check-ups, prescription management, and initial diagnoses. Patients can consult with their primary care physicians from the comfort of their homes, eliminating the need for physical travel and wait times.
This is particularly valuable for managing chronic conditions or seeking guidance on minor health concerns. For example, a patient with a minor respiratory complaint might receive advice on symptom management without leaving their home, giving the sick person more time to rest and reducing the risk of transmission to others.
Specialist consultations
Telehealth transcends geographical constraints, enabling patients to tap into the expertise of specialists without embarking on long and sometimes costly journeys. Individuals facing complex medical issues can virtually consult with specialists, either from their home, or at their local physician’s office, potentially reducing treatment delays and improving outcomes.
For instance, a patient grappling with a rare neurological disorder can receive a second opinion from a renowned specialist located halfway around the world without leaving their hometown.
Mental health support
Telehealth has been a transformative force in the realm of mental health services. Through teletherapy sessions, individuals can access much-needed mental health support from licensed medical professionals. The greater access and discretion afforded by teletherapy can be especially valuable for those who may face stigmas associated with seeking mental health services in person, or who might have specialized needs not served by local counseling resources.
Follow-up care
Telehealth’s benefits can extend into post-surgery or post-discharge scenarios. Patients who have undergone surgical procedures can receive follow-up care virtually, minimizing the need for hospital visits and reducing the risk of missed appointments and/or postoperative complications.
For instance, a patient recovering from joint replacement surgery can have their progress monitored by their surgeon through video consultations, promoting a smoother recovery process.
Examples of telehealth technology
Telehealth is made possible through a diverse array of technologies that enable remote healthcare services to be seamlessly delivered. These innovations in digital healthcare bridge the physical gap between patients and healthcare providers, bringing medical expertise to the digital realm to enhance accessibility and convenience.
Let's explore some key technologies in the telehealth landscape:
Video conferencing
Platforms like Zoom and Microsoft Teams enable real-time, face-to-face consultations between patients and healthcare providers, enabling the delivery of personalized care from a distance.
Mobile apps
Health apps, like Headspace and MyFitnessPal, and wearable devices, like a FitBit or Apple Watch, allow patients to monitor their vital signs, activity levels, and even perform simple tests like glucose monitoring, which can be shared with healthcare professionals.
Remote patient monitoring (RPM)
Remote patient monitoring involves using sensors and devices to collect and transmit patient data to healthcare providers. For example, an individual with cardiac issues might wear a passive heart rate monitoring device or an implanted pacemaker. These technologies can track (and sometimes correct) the patient’s heart rate, while also sending valuable data to their doctor.
Store and forward
The concept of "store and forward" is reshaping healthcare collaboration by allowing patient data, images, videos, and medical records to be shared asynchronously with specialists or consultants. This method is particularly beneficial when immediate responses aren't required but expert insights remain crucial.
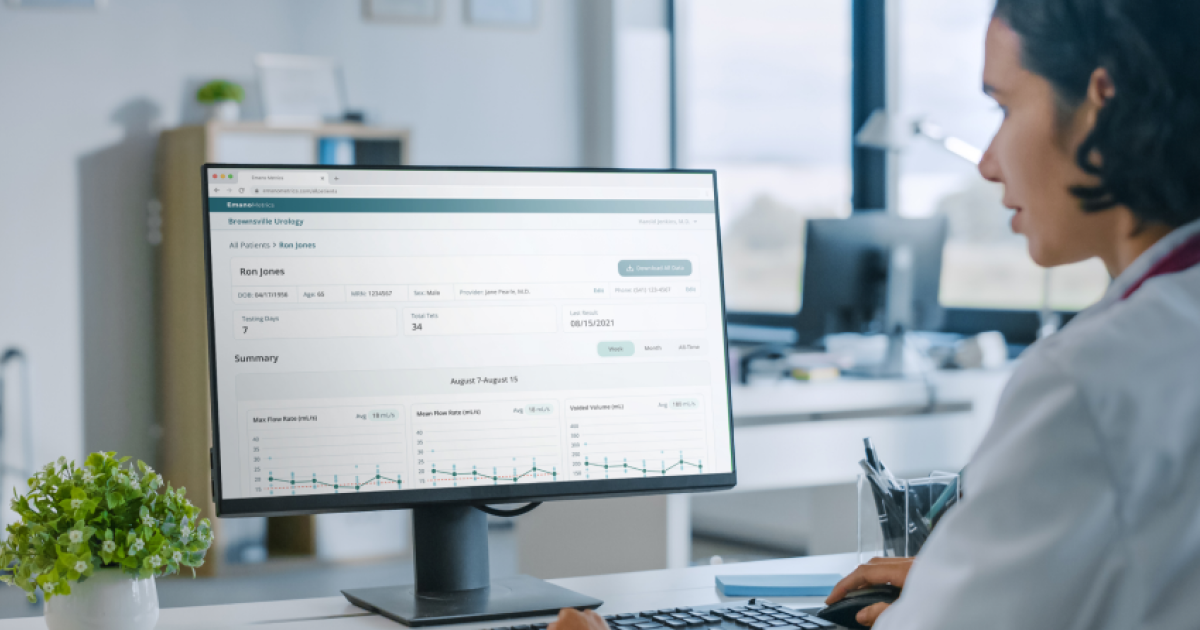
For example, a primary care physician can capture images of a skin condition and send them to a dermatologist for analysis. The dermatologist can review the images and provide insights at their convenience, optimizing the diagnostic process without the need for an in-person visit. Emergent products in this space include Emano Flow, an app that allows urology patients to capture and transmit urinary frequency and volume data to their doctors from home (rather than having to schedule in-office uroflowmetry appointments, as is usually required to diagnose urinary issues).
Final thoughts
The future of healthcare is undeniably intertwined with telehealth. As technology advances, we can expect even more sophisticated ways to remotely monitor patients, share patient medical data securely, and conduct virtual surgeries through robotic assistance. Telehealth has the potential to democratize healthcare, making quality medical services more accessible to populations around the globe.
To learn more about how your healthcare organization can harness the power of telehealth, contact Twenty Ideas - a leading health and med tech design and development agency.
Twenty key ideas from this article
- Overcoming distance barriers, telehealth and telemedicine can reshape healthcare by providing accessible medical services.
- The convergence of technology and healthcare is revolutionizing our approach to seeking, delivering, and encountering medical care.
- Telehealth facilitates remote healthcare delivery through digital tools like video conferencing and data sharing.
- Telehealth can help bridge geographical gaps that can prevent patients from accessing appropriate healthcare resources.
- Focused on remote clinical healthcare, telemedicine spans diagnosis, treatment, and patient management.
- Telemedicine encompasses virtual consultations, prescription management, follow-up care, specialist opinions, chronic condition monitoring, and mental health support.
- While telehealth covers both clinical and non-clinical remote services, telemedicine specializes in remote clinical care.
- Unlocking benefits such as improved access, convenience, cost savings, and enhanced chronic disease management, telehealth can smooth out health care demand and delivery.
- Eliminating distance barriers, telehealth grants remote patients specialized care access.
- Telehealth can improve follow-up visit and medication compliance by providing easier access to medical guidance, prescriptions, and follow-up, saving time and travel.
- By reducing expenses including travel, work absence, and healthcare overhead, telehealth can reduce costs for patients and providers.
- Utilizing Remote Patient Monitoring (RPM), vital signs are tracked through devices, sending data for timely interventions in chronic conditions.
- Telehealth strategically diverts non-emergency cases, optimizing healthcare resources and relieving system loads.
- Leading use cases for telehealth include primary care, specialist opinions, mental health support, and post-treatment care.
- When it comes to primary care, telehealth introduces remote check-ups, prescriptions, and diagnoses.
- Overcoming geographical barriers, telehealth can connect patients with specialists for expert opinions.
- Via virtual sessions, teletherapy offers easily accessible mental health support.
- Expanding care beyond treatment, telehealth's virtual follow-ups curtail hospital visits.
- Emerging trends in telehealth include advanced remote monitoring, secure data sharing, and robot-assisted surgeries.
- Embracing telehealth is the catalyst for transforming healthcare, boosting patient care and accessibility. For expert guidance, reach out to Twenty Ideas - your partner in design and development excellence.





























